Web page, R. L. et al. Medical marijuana, leisure hashish, and cardiovascular well being: a scientific assertion from the American Coronary heart Affiliation. Circulation 142, e131–e152 (2020).
Chandy, M. et al. Adversarial affect of hashish on human well being. Annu. Rev. Med. 75, 353–367 (2024).
Bridgeman, M. B. & Abazia, D. T. Medicinal hashish: historical past, pharmacology, and implications for the acute care setting. P T 42, 180–188 (2017).
Ryan, J. E., McCabe, S. E. & Boyd, C. J. Medicinal hashish: coverage, sufferers, and suppliers. Coverage Polit. Nurs. Pract. 22, 126–133 (2021).
Hoffman, A. F. & Lupica, C. R. Synaptic targets of Δ9-tetrahydrocannabinol within the central nervous system. Chilly Spring Harb. Perspect. Med. 3, a012237 (2013).
Krishna Kumar, Ok. et al. Construction of a signaling cannabinoid receptor 1-G protein complicated. Cell 176, 448–458.e12 (2019).
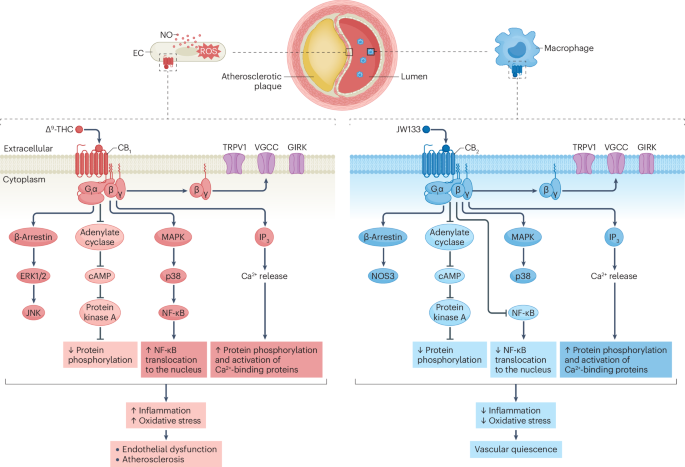
Sugamura, Ok. et al. Activated endocannabinoid system in coronary artery illness and antiinflammatory results of cannabinoid 1 receptor blockade on macrophages. Circulation 119, 28–36 (2009).
Netherland, C. D., Pickle, T. G., Bales, A. & Thewke, D. P. Cannabinoid receptor kind 2 (CB2) deficiency alters atherosclerotic lesion formation in hyperlipidemic Ldlr-null mice. Atherosclerosis 213, 102–108 (2010).
Hoyer, F. F. et al. Atheroprotection through cannabinoid receptor-2 is mediated by circulating and vascular cells in vivo. J. Mol. Cell Cardiol. 51, 1007–1014 (2011).
Pacher, P., Steffens, S., Haskó, G., Schindler, T. H. & Kunos, G. Cardiovascular results of marijuana and artificial cannabinoids: the nice, the unhealthy, and the ugly. Nat. Rev. Cardiol. 15, 151–166 (2018).
Whiting, P. F. et al. Cannabinoids for medical use: a scientific assessment and meta-analysis. JAMA 313, 2456–2473 (2015).
Bilbao, A. & Spanagel, R. Medical cannabinoids: a pharmacology-based systematic assessment and meta-analysis for all related medical indications. BMC Med. 20, 259 (2022).
Bicket, M. C., Stone, E. M. & McGinty, E. E. Use of hashish and different ache remedies amongst adults with persistent ache in US states with medical hashish packages. JAMA Netw. Open. 6, e2249797 (2023).
Zehra, A. et al. Hashish habit and the mind: a assessment. J. Neuroimmune Pharmacol. 13, 438–452 (2018).
Secades-Villa, R., Garcia-Rodriguez, O., Jin, C. J., Wang, S. & Blanco, C. Likelihood and predictors of the hashish gateway impact: a nationwide examine. Int. J. Drug. Coverage 26, 135–142 (2015).
Volkow, N. D., Baler, R. D., Compton, W. M. & Weiss, S. R. Adversarial well being results of marijuana use. N. Engl. J. Med. 370, 2219–2227 (2014).
Wei, T. T. et al. Cannabinoid receptor 1 antagonist genistein attenuates marijuana-induced vascular irritation. Cell 185, 1676–1693.e23 (2022).
DeFilippis, E. M. et al. Cocaine and marijuana use amongst younger adults with myocardial infarction. J. Am. Coll. Cardiol. 71, 2540–2551 (2018).
Patton, D. V. A historical past of United States hashish legislation. J. Legislation Well being 34, 1–29 (2020).
Corridor, W. et al. Public well being implications of legalising the manufacturing and sale of hashish for medicinal and leisure use. Lancet 394, 1580–1590 (2019).
Mead, A. Authorized and regulatory points governing hashish and cannabis-derived merchandise in america. Entrance. Plant. Sci. 10, 697 (2019).
Lampe, J. R. Authorized penalties of rescheduling marijuana. Congressional Analysis Service crsreports.congress.gov/product/pdf/LSB/LSB11105 (2024).
Shirah, B. H., Ahmed, M. M. & Saleh, R. A. in Medicinal Utilization of Hashish and Cannabinoids (eds Preedy, V. R., Patel, V. B. & Martin, C. R.) Ch. 5, 51–61 (Tutorial Press, 2023).
Bahji, A. & Stephenson, C. Worldwide views on the implications of hashish legalization: a scientific assessment & thematic evaluation. Int. J. Env. Res. Public. Well being 16, 3095 (2019).
Rotermann, M. What has modified since hashish was legalized? Well being Rep. 31, 11–20 (2020).
Martins, S. S. et al. Racial and ethnic variations in hashish use following legalization in US states with medical hashish legal guidelines. JAMA Netw. Open. 4, e2127002 (2021).
Chemtob, D. Forbes Each day: The Budding $28B Hemp Market’s Feud with Marijuana. Forbes www.forbes.com/websites/daniellechemtob/2024/04/19/forbes-daily-the-budding-28b-hemp-markets-feud-with-marijuana/ (2024).
Fischer, B., Jutras-Aswad, D. & Corridor, W. Outcomes related to nonmedical hashish legalization coverage in Canada: taking inventory on the 5-year mark. CMAJ 195, E1351–E1353 (2023).
Chong, W. W., Acar, Z. I., West, M. L. & Wong, F. A scoping assessment on the medical and leisure use of hashish in the course of the COVID-19 pandemic. Hashish Cannabinoid Res. 7, 591–602 (2022).
Mackie, Ok. Cannabinoid receptors as therapeutic targets. Annu. Rev. Pharmacol. Toxicol. 46, 101–122 (2006).
Movahed, P. et al. Vascular results of anandamide and N-acylvanillylamines within the human forearm and pores and skin microcirculation. Br. J. Pharmacol. 146, 171–179 (2005).
Pacher, P., Batkai, S. & Kunos, G. Cardiovascular pharmacology of cannabinoids. Handb. Exp. Pharmacol. 599-625 (2005).
Pacher, P., Batkai, S. & Kunos, G. Blood stress regulation by endocannabinoids and their receptors. Neuropharmacology 48, 1130–1138 (2005).
Batkai, S. et al. Endocannabinoids performing at CB1 receptors mediate the cardiac contractile dysfunction in vivo in cirrhotic rats. Am. J. Physiol. Coronary heart Circ. Physiol 293, H1689–H1695 (2007).
Valenta, I. et al. Feasibility analysis of myocardial cannabinoid kind 1 receptor imaging in weight problems: a translational strategy. JACC Cardiovasc. Imaging 11, 320–332 (2018).
Rajesh, M. et al. Cannabinoid 1 receptor promotes cardiac dysfunction, oxidative stress, irritation, and fibrosis in diabetic cardiomyopathy. Diabetes 61, 716–727 (2012).
Mukhopadhyay, P. et al. Pharmacological inhibition of CB1 cannabinoid receptor protects towards doxorubicin-induced cardiotoxicity. J. Am. Coll. Cardiol. 50, 528–536 (2007).
Mukhopadhyay, P. et al. CB1 cannabinoid receptors promote oxidative stress and cell demise in murine fashions of doxorubicin-induced cardiomyopathy and in human cardiomyocytes. Cardiovasc. Res. 85, 773–784 (2010).
Rajesh, M. et al. Cannabinoid receptor 2 activation alleviates diabetes-induced cardiac dysfunction, irritation, oxidative stress, and fibrosis. Geroscience 44, 1727–1741 (2022).
Matyas, C. et al. Interaction of liver–coronary heart inflammatory axis and cannabinoid 2 receptor signaling in an experimental mannequin of hepatic cardiomyopathy. Hepatology 71, 1391–1407 (2020).
Molica, F. et al. Cannabinoid receptor CB2 protects towards balloon-induced neointima formation. Am. J. Physiol. Coronary heart Circ. Physiol 302, H1064–H1074 (2012).
Koivisto, A. P., Belvisi, M. G., Gaudet, R. & Szallasi, A. Advances in TRP channel drug discovery: from goal validation to medical research. Nat. Rev. Drug. Discov. 21, 41–59 (2022).
Pertwee, R. G. Receptors and channels focused by artificial cannabinoid receptor agonists and antagonists. Curr. Med. Chem. 17, 1360–1381 (2010).
Després, J. P., Golay, A. & Sjöström, L. Rimonabant in Weight problems-Lipids Examine Group Results of rimonabant on metabolic danger elements in chubby sufferers with dyslipidemia. N. Engl. J. Med. 353, 2121–2134 (2005).
Onakpoya, I. J., Heneghan, C. J. & Aronson, J. Ok. Worldwide withdrawal of medicinal merchandise due to antagonistic drug reactions: a scientific assessment and evaluation. Crit. Rev. Toxicol. 46, 477–489 (2016).
Cinar, R., Iyer, M. R. & Kunos, G. The therapeutic potential of second and third era CB1R antagonists. Pharmacol. Ther. 208, 107477 (2020).
Crater, G. D., Lalonde, Ok., Ravenelle, F., Harvey, M. & Despres, J. P. Results of CB1R inverse agonist, INV-202, in sufferers with options of metabolic syndrome. A randomized, placebo-controlled, double-blind part 1b examine. Diabetes Obes. Metab. 26, 642–649 (2024).
Hashiesh, H. M., Sharma, C., Goyal, S. N., Jha, N. Ok. & Ojha, S. Pharmacological properties, therapeutic potential and molecular mechanisms of JWH133, a CB2 receptor-selective agonist. Entrance. Pharmacol. 12, 702675 (2021).
Kosar, M. et al. Patent assessment of cannabinoid receptor kind 2 (CB2R) modulators (2016–current). Knowledgeable. Opin. Ther. Pat. 34, 665–700 (2024).
Smoum, R. et al. Editorial: therapeutic potential of the cannabinoid CB2 receptor. Entrance. Pharmacol. 13, 1039564 (2022).
Morales, P., Hernandez-Folgado, L., Goya, P. & Jagerovic, N. Cannabinoid receptor 2 (CB2) agonists and antagonists: a patent replace. Knowledgeable. Opin. Ther. Pat. 26, 843–856 (2016).
Oparil, S. et al. Hypertension. Nat. Rev. Dis. Primers 4, 18014 (2018).
Alshaarawy, O. & Elbaz, H. A. Hashish use and blood stress ranges: United States Nationwide Well being and Vitamin Examination Survey, 2005–2012. J. Hypertens. 34, 1507–1512 (2016).
Golosova, D., Levchenko, V., Kravtsova, O., Palygin, O. & Staruschenko, A. Acute and long-term results of cannabinoids on hypertension and kidney harm. Sci. Rep. 12, 6080 (2022).
Sultan, S. R., Millar, S. A., O’Sullivan, S. E. & England, T. J. A scientific assessment and meta-analysis of the in vivo haemodynamic results of Δ8-tetrahydrocannabinol. Prescription drugs 11, 13 (2018).
Intengan, H. D. & Schiffrin, E. L. Construction and mechanical properties of resistance arteries in hypertension: function of adhesion molecules and extracellular matrix determinants. Hypertension 36, 312–318 (2000).
Corroon, J., Grant, I., Bradley, R. & Allison, M. A. Traits in hashish use, blood stress, and hypertension in middle-aged adults: findings from NHANES, 2009–2018. Am. J. Hypertens. 36, 651–659 (2023).
Vallee, A. Affiliation between hashish use and blood stress ranges in keeping with comorbidities and socioeconomic standing. Sci. Rep. 13, 2069 (2023).
Batkai, S. et al. Endocannabinoids performing at cannabinoid-1 receptors regulate cardiovascular operate in hypertension. Circulation 110, 1996–2002 (2004).
Godlewski, G. et al. Inhibitor of fatty acid amide hydrolase normalizes cardiovascular operate in hypertension with out antagonistic metabolic results. Chem. Biol. 17, 1256–1266 (2010).
Wagner, J. A. et al. Activation of peripheral CB1 cannabinoid receptors in haemorrhagic shock. Nature 390, 518–521 (1997).
Varga, Ok., Wagner, J. A., Bridgen, D. T. & Kunos, G. Platelet- and macrophage-derived endogenous cannabinoids are concerned in endotoxin-induced hypotension. FASEB J. 12, 1035–1044 (1998).
Batkai, S. et al. Endocannabinoids performing at vascular CB1 receptors mediate the vasodilated state in superior liver cirrhosis. Nat. Med. 7, 827–832 (2001).
Ros, J. et al. Endogenous cannabinoids: a brand new system concerned within the homeostasis of arterial stress in experimental cirrhosis within the rat. Gastroenterology 122, 85–93 (2002).
Shan, R. et al. Activation of cannabinoid kind 2 receptor in microglia reduces neuroinflammation by means of inhibiting cardio glycolysis to alleviate hypertension. Biomolecules 14, 333 (2024).
Guo, Y. et al. Cannabidiol protects towards acute aortic dissection by inhibiting macrophage infiltration and PMAIP1-induced vascular easy muscle cell apoptosis. J. Mol. Cell Cardiol. 189, 38–51 (2024).
Curioni, C. & Andre, C. Rimonabant for chubby or weight problems. Cochrane Database Syst. Rev. 2006, CD006162 (2006).
Vidot, D. C. et al. Metabolic syndrome amongst marijuana customers in america: an evaluation of Nationwide Well being and Vitamin Examination Survey knowledge. Am. J. Med. 129, 173–179 (2016).
Mousavi, S. E., Tondro Anamag, F. & Sanaie, S. Affiliation between hashish use and danger of diabetes mellitus kind 2: a scientific assessment and meta-analysis. Phytother. Res. 37, 5092–5108 (2023).
Ravi, D., Ghasemiesfe, M., Korenstein, D., Cascino, T. & Keyhani, S. Associations between marijuana use and cardiovascular danger elements and outcomes: a scientific assessment. Ann. Intern. Med. 168, 187–194 (2018).
Despres, J. P. et al. Impact of rimonabant on the high-triglyceride/low-HDL-cholesterol dyslipidemia, intraabdominal adiposity, and liver fats: the ADAGIO-Lipids trial. Arterioscler. Thromb. Vasc. Biol. 29, 416–423 (2009).
Muniyappa, R. et al. Metabolic results of persistent hashish smoking. Diabetes Care 36, 2415–2422 (2013).
Casier, I., Vanduynhoven, P., Haine, S., Vrints, C. & Jorens, P. G. Is current hashish use related to acute coronary syndromes? An illustrative case sequence. Acta Cardiol. 69, 131–136 (2014).
Jeffers, A. M., Glantz, S., Byers, A. L. & Keyhani, S. Affiliation of hashish use with cardiovascular outcomes amongst US adults. J. Am. Coronary heart Assoc. 13, e030178 (2024).
Frost, L., Mostofsky, E., Rosenbloom, J. I., Mukamal, Ok. J. & Mittleman, M. A. Marijuana use and long-term mortality amongst survivors of acute myocardial infarction. Am. Coronary heart J. 165, 170–175 (2013).
Libby, P. Irritation in atherosclerosis. Nature 420, 868–8743 (2002).
Rajesh, M. et al. Cannabinoid-1 receptor activation induces reactive oxygen species-dependent and -independent mitogen-activated protein kinase activation and cell demise in human coronary artery endothelial cells. Br. J. Pharmacol. 160, 688–700 (2010).
El-Remessy, A. B. et al. Cannabinoid 1 receptor activation contributes to vascular irritation and cell demise in a mouse mannequin of diabetic retinopathy and a human retinal cell line. Diabetologia 54, 1567–1578 (2011).
Paik, D. T., Chandy, M. & Wu, J. C. Affected person and disease-specific induced pluripotent stem cells for discovery of customized cardiovascular medication and therapeutics. Pharmacol. Rev. 72, 320–342 (2020).
Yang, Z., Kulkarni, Ok., Zhu, W. & Hu, M. Bioavailability and pharmacokinetics of genistein: mechanistic research on its ADME. Anticancer. Brokers Med. Chem. 12, 1264–1280 (2012).
Dol-Gleizes, F. et al. Rimonabant, a selective cannabinoid CB1 receptor antagonist, inhibits atherosclerosis in LDL receptor-deficient mice. Arterioscler. Thromb. Vasc. Biol. 29, 12–18 (2009).
Steffens, S. et al. Low dose oral cannabinoid remedy reduces development of atherosclerosis in mice. Nature 434, 782–786 (2005).
Perez-Reyes, M., Owens, S. M. & Di Guiseppi, S. The medical pharmacology and dynamics of marihuana cigarette smoking. J. Clin. Pharmacol. 21, 201S–207S (1981).
Huestis, M. A. Human cannabinoid pharmacokinetics. Chem. Biodivers. 4, 1770–1804 (2007).
Holt, A. et al. Hashish for persistent ache: cardiovascular security in a nationwide Danish examine. Eur. Coronary heart J. 45, 475–484 (2024).
Patel, R. S., Gonzalez, M. D., Ajibawo, T. & Baweja, R. Hashish use dysfunction and elevated danger of arrhythmia-related hospitalization in younger adults. Am. J. Addict. 30, 578–584 (2021).
Chouairi, F. et al. Hashish use dysfunction amongst atrial fibrillation admissions, 2008-2018. Pacing Clin. Electrophysiol. 44, 1934–1938 (2021).
Gillett, L. et al. Arrhythmic results of hashish in ischemic coronary heart illness. Hashish Cannabinoid Res. 8, 867–876 (2023).
Richards, J. R. Mechanisms for the danger of acute coronary syndrome and arrhythmia related to phytogenic and artificial cannabinoid use. J. Cardiovasc. Pharmacol. Ther. 25, 508–522 (2020).
Kariyanna, P. T. et al. Marijuana induced myocarditis: a brand new entity of poisonous myocarditis. Am. J. Med. Case Rep. 6, 169–172 (2018).
Khanji, M. Y. et al. Affiliation between leisure hashish use and cardiac construction and performance. JACC Cardiovasc. Imaging 13, 886–888 (2020).
Bene-Alhasan, Y. et al. Each day marijuana use is related to incident coronary heart failure: “All of Us” analysis program [abstract]. Circulation 148 (Suppl. 1), 13812 (2023).
Chen, B. et al. Endothelial cannabinoid CB1 receptor deficiency reduces arterial irritation and lipid uptake in response to atheroprone shear stress. Preprint at bioRxiv, https://doi.org/10.1101/2024.05.15.594375 (2024).
Mukhopadhyay, P. et al. Fatty acid amide hydrolase is a key regulator of endocannabinoid-induced myocardial tissue harm. Free. Radic. Biol. Med. 50, 179–195 (2011).
Slavic, S. et al. Cannabinoid receptor 1 inhibition improves cardiac operate and remodelling after myocardial infarction and in experimental metabolic syndrome. J. Mol. Med. 91, 811–823 (2013).
Defer, N. et al. The cannabinoid receptor kind 2 promotes cardiac myocyte and fibroblast survival and protects towards ischemia/reperfusion-induced cardiomyopathy. FASEB J. 23, 2120–2130 (2009).
McPartland, J. M., Duncan, M., Di Marzo, V. & Pertwee, R. G. Are cannabidiol and Δ9-tetrahydrocannabivarin adverse modulators of the endocannabinoid system? A scientific assessment. Br. J. Pharmacol. 172, 737–753 (2015).
Alfulaij, N. et al. Cannabinoids, the center of the matter. J. Am. Coronary heart Assoc. 7, e009099 (2018).
Lee, W. S. et al. Cannabidiol limits T cell-mediated persistent autoimmune myocarditis: implications to autoimmune issues and organ transplantation. Mol. Med. 22, 136–146 (2016).
Hao, E. et al. Cannabidiol protects towards doxorubicin-induced cardiomyopathy by modulating mitochondrial operate and biogenesis. Mol. Med. 21, 38–45 (2015).
Rajesh, M. et al. Cannabidiol attenuates cardiac dysfunction, oxidative stress, fibrosis, and inflammatory and cell demise signaling pathways in diabetic cardiomyopathy. J. Am. Coll. Cardiol. 56, 2115–2125 (2010).
Hampson, A. J., Grimaldi, M., Axelrod, J. & Wink, D. Cannabidiol and (–)Δ9-tetrahydrocannabinol are neuroprotective antioxidants. Proc. Natl Acad. Sci. USA 95, 8268–8273 (1998).
Pacher, P., Kogan, N. M. & Mechoulam, R. Past THC and endocannabinoids. Annu. Rev. Pharmacol. Toxicol. 60, 637–659 (2020).
Gonca, E. & Darici, F. The impact of cannabidiol on ischemia/reperfusion-induced ventricular arrhythmias: the function of adenosine A1 receptors. J. Cardiovasc. Pharmacol. Ther. 20, 76–83 (2015).
Stanley, C. P., Hind, W. H., Tufarelli, C. & O’Sullivan, S. E. Cannabidiol causes endothelium-dependent vasorelaxation of human mesenteric arteries through CB1 activation. Cardiovasc. Res. 107, 568–578 (2015).
Kumric, M., Bozic, J., Dujic, G., Vrdoljak, J. & Dujic, Z. Power results of efficient oral cannabidiol supply on 24-h ambulatory blood stress and vascular outcomes in handled and untreated hypertension (HYPER-H21-4): examine protocol for a randomized, placebo-controlled, and crossover examine. J. Pers. Med. 12, 1037 (2022).
Nationwide Convention of State Legislatures. State Medical Hashish Legal guidelines NCSL www.ncsl.org/well being/state-medical-cannabis-laws (2024).
Balachandran, P., Elsohly, M. & Hill, Ok. P. Cannabidiol interactions with drugs, illicit substances, and alcohol: a complete assessment. J. Gen. Intern. Med. 36, 2074–2084 (2021).
Moore, A., Straube, S., Fisher, E. & Eccleston, C. Cannabidiol (CBD) merchandise for ache: ineffective, costly, and with potential harms. J. Ache 25, 833–842 (2024).
Bhat, T. A., Kalathil, S. G., Goniewicz, M. L., Hutson, A. & Thanavala, Y. Not all vaping is similar: differential pulmonary results of vaping cannabidiol versus nicotine. Thorax 78, 922–932 (2023).
Rossheim, M. E., LoParco, C. R., Henry, D., Trangenstein, P. J. & Walters, S. T. Delta-8, delta-10, HHC, THC-O, THCP, and THCV: what ought to we name these merchandise? J. Stud. Alcohol. Medication 84, 357–360 (2023).
O’Mahony, B., O’Malley, A., Kerrigan, O. & McDonald, C. HHC-induced psychosis: a case sequence of psychotic sickness triggered by a extensively out there semisynthetic cannabinoid. Ir. J. Psychol. Med. https://doi.org/10.1017/ipm.2024.3 (2024).
Harlow, A. F., Miech, R. A. & Leventhal, A. M. Adolescent Δ8-THC and marijuana use within the US. JAMA 331, 861–865 (2024).
Govindarajan, R. Ok. et al. Biosynthesis of phytocannabinoids and structural insights: a assessment. Metabolites 13, 442 (2023).
Raup-Konsavage, W. M. et al. Environment friendly synthesis for altering facet chain size on cannabinoid molecules and their results in chemotherapy and chemotherapeutic induced neuropathic ache. Biomolecules 12, 1869 (2022).
Nachnani, R., Raup-Konsavage, W. M. & Vrana, Ok. E. The pharmacological case for cannabigerol. J. Pharmacol. Exp. Ther. 376, 204–212 (2021).
Peters, E. N. et al. Pharmacokinetics of cannabichromene in a medical hashish product additionally containing cannabidiol and Δ9-tetrahydrocannabinol: a pilot examine. Eur. J. Clin. Pharmacol. 78, 259–265 (2022).
Abioye, A. et al. Δ9-Tetrahydrocannabivarin (THCV): a commentary on potential therapeutic profit for the administration of weight problems and diabetes. J. Hashish Res. 2, 6 (2020).
Jadoon, Ok. A. et al. Efficacy and security of cannabidiol and tetrahydrocannabivarin on glycemic and lipid parameters in sufferers with kind 2 diabetes: a randomized, double-blind, placebo-controlled, parallel group pilot examine. Diabetes Care 39, 1777–1786 (2016).
Dziemitko, S., Harasim-Symbor, E. & Chabowski, A. How do phytocannabinoids have an effect on cardiovascular well being? An replace on the commonest cardiovascular illnesses. Ther. Adv. Power Dis. 14, 20406223221143239 (2023).
DeFilippis, E. M. et al. Marijuana use in sufferers with heart problems: JACC assessment matter of the week. J. Am. Coll. Cardiol. 75, 320–332 (2020).
Bedi, G., Cooper, Z. D. & Haney, M. Subjective, cognitive and cardiovascular dose-effect profile of nabilone and dronabinol in marijuana people who smoke. Addict. Biol. 18, 872–881 (2013).
Zongo, A. et al. Medical hashish authorization and the danger of cardiovascular occasions: a longitudinal cohort examine. BMC Cardiovasc. Disord. 21, 426 (2021).
Devinsky, O. et al. Impact of cannabidiol on drop seizures within the Lennox–Gastaut syndrome. N. Engl. J. Med. 378, 1888–1897 (2018).
Devinsky, O. et al. Trial of cannabidiol for drug-resistant seizures within the Dravet syndrome. N. Engl. J. Med. 376, 2011–2020 (2017).
Ahmed, A. et al. Results of digoxin at low serum concentrations on mortality and hospitalization in coronary heart failure: a propensity-matched examine of the DIG trial. Int. J. Cardiol. 123, 138–146 (2008).
Lee, Ok. et al. Cannabidiol publicity throughout gestation results in antagonistic cardiac outcomes early in postnatal life in male rat offspring. Hashish Cannabinoid Res. 9, 781–796 (2024).
D’hooghe, M. et al. Sativex(R) (nabiximols) cannabinoid oromucosal spray in sufferers with resistant a number of sclerosis spasticity: the Belgian expertise. BMC Neurol. 21, 227 (2021).
Nurmikko, T. J. et al. Sativex efficiently treats neuropathic ache characterised by allodynia: a randomised, double-blind, placebo-controlled medical trial. Ache 133, 210–220 (2007).
Adams, A. J. et al. “Zombie” outbreak attributable to the artificial cannabinoid AMB-FUBINACA in New York. N. Engl. J. Med. 376, 235–242 (2017).
Fantegrossi, W. E., Moran, J. H., Radominska-Pandya, A. & Prather, P. L. Distinct pharmacology and metabolism of K2 artificial cannabinoids in comparison with Δ9-THC: mechanism underlying larger toxicity? Life Sci. 97, 45–54 (2014).
Hermanns-Clausen, M. et al. Acute negative effects after consumption of the brand new artificial cannabinoids AB-CHMINACA and MDMB-CHMICA. Clin. Toxicol. 56, 404–411 (2018).
Mir, A., Obafemi, A., Younger, A. & Kane, C. Myocardial infarction related to use of the artificial cannabinoid K2. Pediatrics 128, e1622–e1627 (2011).
Jayakumar, N. et al. Co-use and mixing tobacco with hashish amongst Ontario adults. Nicotine Tob. Res. 23, 171–178 (2021).
Wu, T. C., Tashkin, D. P., Djahed, B. & Rose, J. E. Pulmonary hazards of smoking marijuana as in contrast with tobacco. N. Engl. J. Med. 318, 347–351 (1988).
Hancox, R. J. et al. Results of hashish on lung operate: a population-based cohort examine. Eur. Respir. J. 35, 42–47 (2010).
Tan, W. C. et al. The results of marijuana smoking on lung operate in older individuals. Eur. Respir. J. 54, 1900826 (2019).
Crosland, B. A. et al. Threat of antagonistic neonatal outcomes after mixed prenatal hashish and nicotine publicity. JAMA Netw. Open. 7, e2410151 (2024).
Hammond, C. J. et al. Co-occurring tobacco and hashish use in adolescents: dissociable relationships with mediofrontal electrocortical exercise throughout reward suggestions processing. Neuroimage Clin. 30, 102592 (2021).
Vogel, E. A., Rubinstein, M. L., Prochaska, J. J. & Ramo, D. E. Associations between marijuana use and tobacco cessation outcomes in younger adults. J. Subst. Abuse Deal with. 94, 69–73 (2018).
Panlilio, L. V., Solinas, M., Matthews, S. A. & Goldberg, S. R. Earlier publicity to THC alters the reinforcing efficacy and anxiety-related results of cocaine in rats. Neuropsychopharmacology 32, 646–657 (2007).
Bierut, L. J. et al. Familial transmission of substance dependence: alcohol, marijuana, cocaine, and recurring smoking: a report from the Collaborative Examine on the Genetics of Alcoholism. Arch. Gen. Psychiatry 55, 982–988 (1998).
Hartz, S. M. et al. Elevated genetic vulnerability to smoking at CHRNA5 in early-onset people who smoke. Arch. Gen. Psychiatry 69, 854–860 (2012).
Lubke, G. H., Stephens, S. H., Lessem, J. M., Hewitt, J. Ok. & Ehringer, M. A. The CHRNA5/A3/B4 gene cluster and tobacco, alcohol, hashish, inhalants and different substance use initiation: replication and new findings utilizing combination analyses. Behav. Genet. 42, 636–646 (2012).
Ibsen, M. S., Connor, M. & Glass, M. Cannabinoid CB1 and CB2 receptor signaling and bias. Hashish Cannabinoid Res. 2, 48–60 (2017).
Cheung, C. P. et al. Hashish inhalation acutely reduces muscle sympathetic nerve exercise in people. Circulation 146, 1972–1974 (2022).