How Neuroscience Is Changing the Way We Treat Depression
Depression is a complex mental health condition affecting millions worldwide. Traditionally, treatments such as psychotherapy and antidepressants have been the cornerstones of care. However, advances in neuroscience are revolutionizing how we understand and treat this debilitating condition, offering new hope to those who struggle. This article explores groundbreaking developments in neuroscience that are reshaping depression treatment.
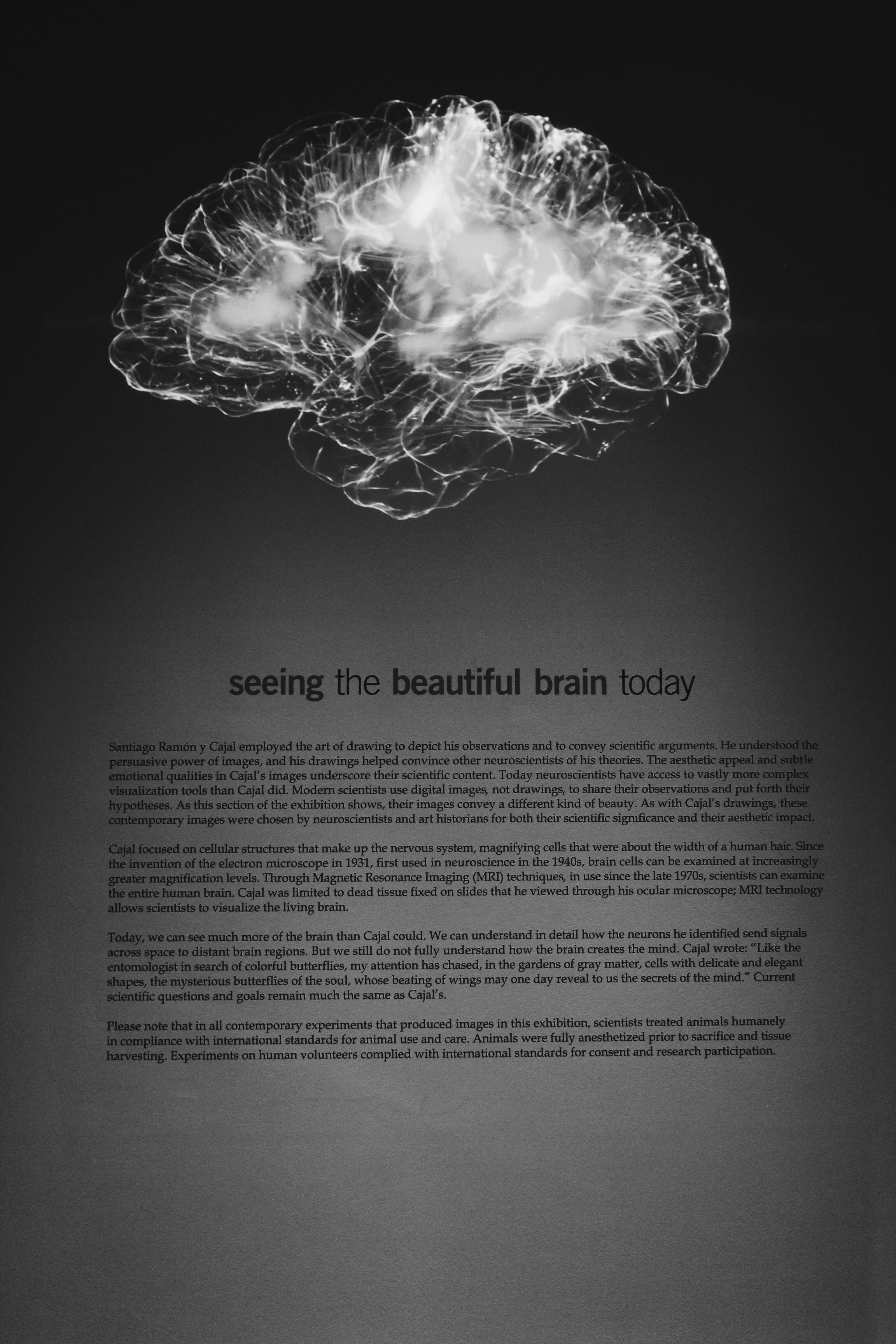
The Neuroscience of Depression
Depression is no longer viewed solely as a “chemical imbalance” in the brain. Neuroscientific research has revealed that depression involves:
-
Altered Brain Connectivity
-
Depressed individuals often exhibit disrupted communication between brain regions, particularly the prefrontal cortex and amygdala, which regulate mood and stress.
-
-
Neuroinflammation
-
Chronic inflammation in the brain can exacerbate depressive symptoms, linking physical health and mental well-being.
-
-
Impaired Neuroplasticity
-
The brain’s ability to adapt and form new connections (neuroplasticity) is often diminished in depression, making it harder for individuals to recover from negative experiences.
-
For an overview of common psychological disorders, visit our article on common psychological disorders and how to recognize them.
Innovative Neuroscience-Based Treatments
Neuroscience is paving the way for innovative, targeted treatments for depression. Here are some of the most promising advancements:
1. Ketamine and Esketamine Therapy
Ketamine, traditionally used as an anesthetic, has emerged as a rapid-acting antidepressant.
How It Works:
-
Ketamine affects glutamate, a neurotransmitter critical for brain plasticity.
-
It promotes rapid synaptic growth, helping to “reset” brain networks disrupted by depression.
Esketamine, a nasal spray version, has been FDA-approved for treatment-resistant depression.
2. Transcranial Magnetic Stimulation (TMS)
TMS is a non-invasive therapy that uses magnetic fields to stimulate nerve cells in the brain.
Key Benefits:
-
Targets specific regions like the dorsolateral prefrontal cortex, implicated in mood regulation.
-
Offers a safe alternative for individuals who don’t respond to traditional treatments.
Learn more about the brain’s adaptability in how cognitive behavioral therapy can change your life.
3. Deep Brain Stimulation (DBS)
Initially developed for Parkinson’s disease, DBS involves implanting electrodes in specific brain regions.
Current Research:
-
DBS shows promise for individuals with severe, treatment-resistant depression.
-
Targets areas like the subgenual cingulate cortex to alleviate depressive symptoms.
4. Psychedelic-Assisted Therapy
Psychedelics such as psilocybin (found in “magic mushrooms”) are being explored for their transformative potential in depression treatment.
Mechanism of Action:
-
Psilocybin promotes neural connectivity and emotional processing.
-
Facilitates profound therapeutic experiences, helping individuals reframe negative thought patterns.
5. Gut-Brain Axis Interventions
Emerging research highlights the role of gut health in mental health.
Findings:
-
The gut microbiome influences brain function through the vagus nerve and inflammatory pathways.
-
Probiotics and dietary changes are being studied as adjunct therapies for depression.
For tips on managing stress, which often coexists with depression, see our article on effective stress management techniques.
Personalized Medicine in Depression Treatment
The one-size-fits-all approach to depression treatment is increasingly being replaced by personalized strategies, thanks to advancements in neuroscience.
Genetic Testing:
-
Identifying genetic markers can help tailor antidepressant selection and dosage.
Biomarkers:
-
Brain imaging and blood tests may predict treatment response, reducing the trial-and-error period for patients.
Digital Therapeutics:
-
Apps and wearable devices are being developed to monitor symptoms and deliver real-time interventions.
Challenges and Ethical Considerations
While neuroscience offers groundbreaking possibilities, challenges remain:
-
Accessibility: High costs may limit access to advanced treatments like TMS or DBS.
-
Long-Term Effects: The safety and efficacy of emerging therapies like psychedelics require further study.
-
Ethical Concerns: Technologies like brain implants raise questions about autonomy and consent.
The Future of Depression Treatment
As neuroscience continues to evolve, so does the potential for more effective, targeted treatments for depression. The integration of brain imaging, genetic testing, and innovative therapies is shaping a future where depression care is more precise, accessible, and transformative.
For further reading on understanding mental health, visit our article on depression.